
Opportunities for Employers to Lead – Stopping the Spread of COVID-19 Webinar Recap
The Alliance, Business Health Care Group (BHCG), and WEA Trust and Health Tradition Health Plan were pleased to host a webinar with the University of Wisconsin-Madison Population Health Institute on Dec. 10. The webinar featured Dr. Jon Meiman, Chief Medical Officer and State Epidemiologist for Environmental and Occupational Health at the Wisconsin Department of Health Services, and Dr. Robert Meyer, Occupational Medicine Physician for Bellin Health Systems. This is a recap of the virtual event. Click here to view the full recording. External Link. Opens in new window..
Current State of the Pandemic
Dr. Meiman briefly covered Wisconsin’s pandemic status and its strain on our health care system. Hospitals have seen exponentially more cases in the past three months, and when hospitals are full, it impacts the care of all patients. The number of patients hospitalized peaked in Wisconsin, reaching 2,278 on Nov. 16. Another factor Dr. Meiman said we could not overlook is the economic impact the pandemic has caused. Merely looking at unemployment, there’s been a massive spike – which has significantly improved – but there are people and businesses still struggling.
COVID-19 Transmission
Dr Meiman moved to the scientific evidence of how COVID-19 spreads and quickly ran through what we know about the virus thus far.
- It can be contracted from contaminated surfaces.
- After exposure, it can take up to two weeks to develop symptoms.
- Roughly 20% of those infected never develop symptoms but can still spread the virus.
- Spread happens through droplets (from the mouth), covering short distances (less than 6 feet).
However, Dr. Meiman expressed that avoiding close contact – being more than 6-feet apart for less than 15 minutes at a time – may be an oversimplification when considering one’s risk for infection. There’s strong evidence supporting that high-density occupancy, poorly ventilated indoor facilities, and activities like singing or shouting can spread more droplets further. Therefore, avoiding close contact, by definition, is likely insufficient in circumstances where any one of those three elements occur, and extreme caution is encouraged.
Drivers of Transmission:
Dr. Meiman then discussed the three drivers of virus transmission: Within households, in common gathering places, and within workplaces.
He explained that in a recent CDC study conducted in Tennessee and Marshfield, Wisconsin, after a family member of a household tested positive, 53% of all other household members ultimately tested positive. To further illustrate his point, Dr. Meiman showcased a study in Singapore where poor migrant laborers living in dormitories or barracks made up 88% of Singapore’s total cases nationally.
As far as common gathering places and workplaces go, Dr. Meiman pointed out that congregation and close contact poses a risk anywhere, and workplaces can create an environment for the rapid spread of COVID-19 among employees without proper procedures and safeguards in place.
Managing Risk for Employers
Next, Dr. Meyer shifted to talking about what employers can do to manage COVID-19 in the workplace.
He displayed a diagram of The Swiss Cheese Respiratory Virus Pandemic Defense model that employers can deploy to stop a virus. The model recognizes that no single intervention is perfect at preventing the spread of a virus, and although each intervention (each slice of swiss cheese) has imperfections (holes), by using multiple layers of defense, we can improve our chances of successfully defending the spread of the virus.
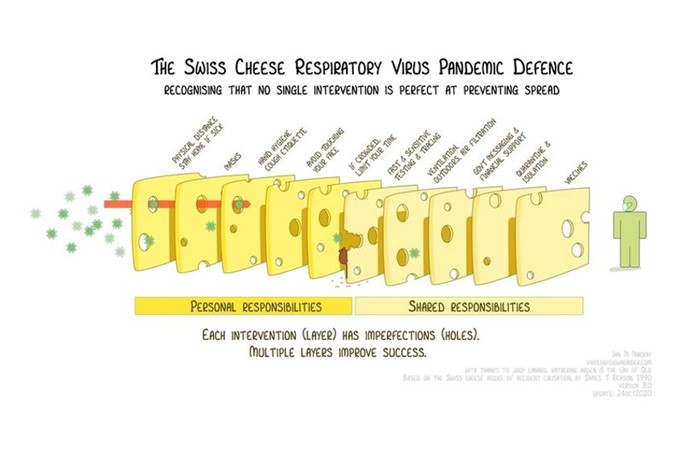
The personal interventions that are proven to help prevent the spread of disease are:
- Physical distancing
- Staying home when ill
- Hand hygiene and cough etiquette
- Avoid/Limit time spent in crowded spaces
The shared interventions proven to help prevent the spread of disease are:
- Swift and sensitive testing and tracing
- Proper ventilation
- Government messaging and financial support
- Quarantine and isolation
- Vaccines
Dr. Meyer ended the model’s discussion by explaining that when individuals, employers, and public health work together, we can use all the intervention tactics in synergy to defeat the virus’ spread.
Providing Critical Employee Education
He then explained that to educate employees, employers should consider a few elements. First, to make sure messaging and educational resources are clear and concise. Employers should also have a firm grasp of the ethnicities of their workforces and ensure communication pieces are made readily available in languages other than English, if necessary. Dr. Meyer then went over a simple checklist for employers to convey to employees consistently:
- Stay home when sick
- Wear a mask at all times (when possible)
- Wash your hands often
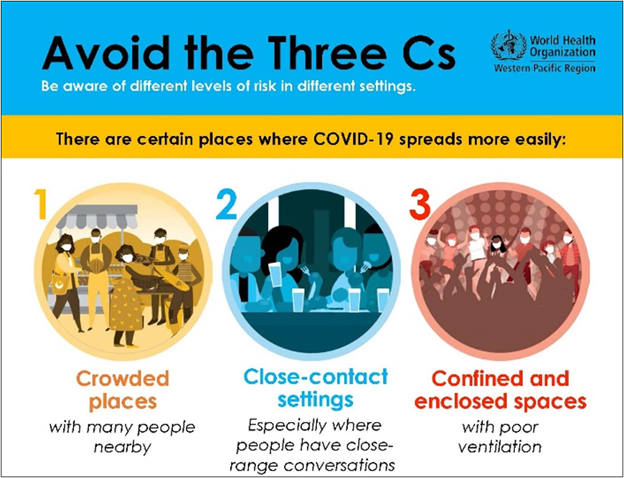
- Keep your distance and avoid the “three C’s”
- Avoid crowded places
- Avoid close-contact settings
- Avoid confined and enclosed spaces
Creating a Safer Work Environment
Dr. Meyer admitted that some businesses might have more trouble than others creating safe spaces, but he believes there’s always something employers can improve on. He outlines four key areas of for employers to pay attention to:
1) Environmental Modifications: Employers can audit their workflows. They can then decide to deploy changes by manipulating their employees’ physical environments to prevent spreading. For example, they can change the distance that separates employees (physical distancing,) install physical barriers (when physical distancing isn’t possible,) upgrade their workplace ventilation systems, and improve their symptom screening system.
2) Universal Masking Requirements: Require employees to wear masks at all times (when feasible).
3) Employee Training and Education: Employers should provide their employees with proper hygiene and protective behavior training in multiple ways as often as possible. They should also equip their employees with appropriate PPE to empower them to do their jobs safely. Employers should have policies and procedures in place, make sure employees know them, and revise as new information comes to light. Further, Dr. Meyer re-emphasized the need for all communication pieces to be written in clear, concise language and in all appropriate languages for their specific workspace.
4) Workplace Policies That Reduce “Presenteeism”: Lastly, Dr. Meyer suggested implementing policies that reduce the occupational transmission risk that employees pose by working while symptomatic. Flexible work policies, like remote work (when possible) is ideal. Providing employees with paid sick leave is also advised, and employers are encouraged to review their “perfect attendance” policies and temporarily suspend or amend incentives for good attendance.
Working With Your Local or Tribal Health Department
Finally, should an employer have someone test positive, they should work with their local or tribal health department (LTHD) to keep their business open. Two or more workers with COVID-19 in 28 days constitute an outbreak investigation, and employers should contact the LTHD as soon as possible to operate the investigation.
Dr. Meyer made clear that “whether or not the outbreak is workplace-related does not change how you work with the LTHD to stop COVID-19 in your workplace. Outbreak investigations are faster and more effective when started quickly. Confidential information will be exchanged and protected as you work with the LTHD to stop the spread.”
Prompt action is necessary for large businesses, and quickly identifying close contacts prevents a small outbreak from spreading uncontrollably.
How Does an Employer Conduct Testing?
Testing in the workplace can be done by a health care provider or community testing site. Testing is critical when trying to manage an outbreak that is rapidly growing. As a quick rule-of-thumb:
- PCR tests are highly accurate, expensive, and the turnaround time can be long
- Antigen testing is cheaper, faster, but also less accurate
For outbreaks: LTHDs will determine the best testing strategy based on the information they have.
For routine testing of employees: work closely with occupational health providers.
Vaccines – When, Where, and How Many?
Pfizer’s vaccine is expected to be authorized soon, while Moderna’s is currently under review. Both vaccines are highly promising, offering over 90% efficacy, and both require two doses.
However, Wisconsin’s initial allotment of vaccines is just under 50,000 doses (or just under 25,000 people), and the CDC vaccine advisory committee (ACIP) is recommending the following groups as priorities for vaccination through three phases:
Phase 1a: Health care personnel and long-term care facility residents.
Phase 1b: Essential workers.
Phase 1c: Adults aged 65+ and adults with high-risk medical conditions.
Dr. Meyer said that regardless of vaccine prioritization, the supply will be extremely limited and its rollout will be logistically complex. In other words, it will take months. So how can employers help? Dr. Meyer suggests promoting vaccination now to help increase public trust in the vaccine, and when the time comes, employers can help facilitate getting vaccines to their workforces.
We Can Stop the Spread Together
Dr. Meyer closed his portion of the webinar with a call for prudence. “More Americans are infected now than ever before, so over the next several months we still need to test, trace, isolate, quarantine, wear masks, and socially distance.”
The webinar concluded with specific employer questions that were answered in the webinar. You can view its recording here. External Link. Opens in new window..








