
2020 Fall Symposium & Annual Meeting Recap
The Alliance hosted their 30th Fall Symposium & Annual Meeting on Thursday, Oct. 1 as on online event. This article recaps the keynote speakers in the latter half of the event, but you can re-watch the event in its entirety here. External Link. Opens in new window..
Employers Are The Key To Unlocking Better Prices
The Alliance invited Chris Whaley, Policy Researcher at RAND Corporation, to discuss the recently released results of their Hospital Price Transparency Study. External Link. Opens in new window.. The study examines the costs that employers pay for hospital prices, benchmarked against Medicare across the United States.
Chris started off his presentation by displaying the sheer magnitude of employer-sponsored health coverage. “Employers cover half of Americans – or 160 million people – with $1.2 trillion in total health care costs in 2018, and $480 billion of that was hospital costs.”
Then he reviewed what we already know about health care: the prices paid by employers are rising much more rapidly than Medicare and Medicaid, and employees are paying more for health care every year, while wages have remained relatively the same.
“These rising health care costs place a tremendous amount of pressure on employers and their populations. This is especially true during the COVID-19 pandemic,” Chris said. In fact, it’s likely that Americans will spend one out of every five dollars. External Link. Opens in new window. on health care in 2021.
Key Takeaways from RAND Corp Study
After level-setting, he delved into the data by showing that commercial prices relative to Medicare have increased from 224% in 2016 to 247% in 2018. In other words, employers are paying 2.5 times more for the same inpatient and outpatient services at hospitals than Medicare – and that disparity continues to grow at a compounded interest rate 5.1% annually.
Next, he showed that, relative to Medicare, commercial prices, facility prices, and professional prices all vary widely across states, within states, and within hospital systems in those states. For example, Wisconsin ranks 3rd highest in professional prices and pays nearly 350% more in that category, while Illinois pays just under 200% more for those same professional services.
More importantly, he showed that there was no correlation between the differences in hospital pricing and “low” government reimbursement for Medicare – what health systems refer to as “uncompensated care” – to account for the variation of prices.
In terms of quality, Chris explained that while there are many high-value hospitals across the country, there’s no real evidence to suggest that safety and quality are commensurate with price. “All the outcomes that health care purchasers value, such as patient convenience and hospital reputation do not show a clear link between hospital price and quality/safety.”
How Employers Can Use RAND Corp Study
“The wide variation in prices for hospital care presents a really important savings opportunity for employers. Employers can use innovations and benefit plan design strategies to save money and get more value for what they’re paying. But employers need to do a better job in demanding transparent information on prices.” Chris went on to say that when employers have transparent information about prices, they can benchmark those prices and demand change from hospital networks.
Chris admitted employers could use some help from state and federal policymakers in that arena: “70% of hospitals are in non-competitive, dominated markets, so if there’s only one or two hospitals in your market it can be tough to demand fairer prices as a smaller employer.”
Despite those obstacles, Chris outlined a few pieces of regulatory reforms employers can push for to improve prices in the future:
- An all-payer claims database that highlights the variation in prices.
- Policies that promote competition and eliminate gag clauses.
- Limits on out-of-network charges and surprise billing.
- All-payer or global budget programs (also known as Total Cost-of-Care Contracting).
- Enroll in RAND 4.0.. External Link. Opens in new window.
Driving High-Value Health Care at The Alliance
The next portion of the Symposium was a presentation by leadership at The Alliance, Melina Kambitsi, Ph.D., and Kyle Monroe, who used the four core drivers of high-value health care to explain how employers who work with The Alliance can work on combating the high prices the RAND study illustrated.
Kyle began by stating simply, “The Alliance believes health care prices should be simple, predictable, and transparent; simple for purchasers and consumers to understand and easy to compare rates from different provider organizations, predictable for costs for services, and transparent with accessible cost and quality information for purchasers.”
Reference-Based Contracting by The Alliance
He went on to say that some organizations are already trying to discredit the RAND study, “They say this is impossible: that benchmarking to Medicare is inappropriate, or Medicare’s methodology is flawed, or that providers will never agree to something like this. Let me be very clear, anyone who says it isn’t possible or that it can’t be done is flat out wrong.”
Why? The Alliance is already doing it with Reference-Based Contracting; more than 80% of our contracts are repriced using referenced-based contracts benchmarked to Medicare. “Using a percentage of Medicare resets the starting point for pricing from billed charge to something with a rational base rate, plus discounts and adjustments.”
Total Cost-of-Care Contracting
Kyle then explained that Reference-Based Contracting – what we’re doing now – leads us to Total Cost-of-Care Contracting – what we’re moving towards. “Medicare-based agreements are a good start, but they are not the end goal. Total-Cost Contracting, also known as global payments, transfers [more of] the financial risk to the providers.”
This method could provide subscription-based fixed payments for patients and force providers to allocate a budget for services, so if they go over budget, that money would come out of the provider’s pocket, not the employer’s. It would also provide robust and transparent data and analytics, more intimate relationships with provider organizations, and incorporate actionable quality data.
The Growth of Smarter Networks℠
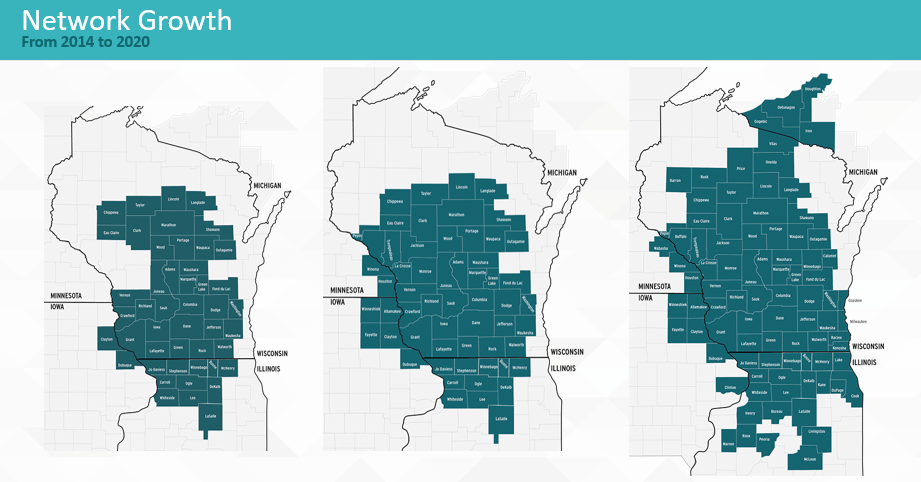
Kyle shifted the focus of his presentation to Smarter Networks by The Alliance. “Our membership is growing so our network has to grow, and we don’t just grow the network for growth’s sake, we only add providers that add value for our members.”
The Alliance designed Smarter Networks as a platform to align incentives for all stakeholders and provide innovative plan design. Employees want options to go to high-quality providers and pay as little as they can, employees and plan sponsors want the best outcomes for the lowest price, and providers want to work with employers. Our networks promote those high-value providers.
The Alliance Premier Network
He then displayed how the latest offering by The Alliance, The Premier Network, is unique in that it reduces costs, removes barriers to care, and promotes high-quality care. “We were able to negotiate rates for providers in the Premier Network that were 15-30% lower than The Alliance Comprehensive Network.”
The Premier Network is a customizable multi-level benefit plan for employers that incentivizes patients to choose high-value providers without limiting their choice.
Melina joined the discussion to explain how tiering in the Premier Network may work using a current member’s network design:
Tier 1 – Non-emergent schedulable procedures and on-site clinic with preferred providers.
Tier 2 – Specialty care and emergency care with secondary preferred providers.
Tier 3 – Wrap Network with other health systems.
Tier 4 – Out-of-Network reference-based pricing with AMPS (another new offering to negotiate with those providers that may be outside The Comprehensive Network by The Alliance)
Achieving Advanced Primary Care
In addition to all the expanding network and new product offerings, Melina talked about the importance of Advanced Primary Care for employers. “We know that care starts at the primary care physician’s office. We also know that over 80% of patients with chronic physicians see their primary care doctor multiple times per year. And because primary care is the least expensive care, the PCP visit has become the most important type of care.”
However, Melina explained that misaligned incentives, lack of behavioral health integration, and lack of appropriate referrals at the primary care level drive up costs, compromise the effectiveness of care, and reduce patient satisfaction. She then went on to explain the characteristics of Advanced Primary Care and how it combats those issues:
Enhanced Access for Patients
More physician-patient time, enhanced scope of services, more immediate care availability, and availability outside of clinic operation hours
Evidence-Based Medicine
Care teams avoid test orders not linked to evidence and change management. Standing orders and protocols for patients with chronic disease management.
Risk-Stratified Care Management
Each patient receives care based on their unique needs: extended office visits, care manager guidance, monitoring, and tracking, phone check-ups, etc.
Care Coordination
Primary care team that engages in outreach, including chronic care condition management; coordination of care; and ensuring patient understanding of medications, orders, adherence expectations, etc.
Care Navigation
Careful selection of specialists – clinicians use a narrow list whom they trust and remain in constant contact as treatment plans develop.
Organizational Infrastructure & Backbone
Analytical and reporting capabilities, EMRs, coordination and communication with other providers, payers, and continuous staff improvement and training.
Behavioral Health Integration
Using patient records, care teams can identify patients who may need outreach to assess behavioral health needs through multiple methods of connection.
Balanced Compensation
Rewarding care management team based on quality of care – care quality, patient experience, resource use and referrals – not volume of care. This global payment methodology differs from traditional primary care, which uses fee-for-service payments and third-party payers.
Referral Management
Fewer referrals outside of the primary care ecosystem.
2020 Health Transformation Awards
The Alliance ended the event with their 30th anniversary video. External Link. Opens in new window. and the announcement of the 2020 Health Transformation Award Winners. External Link. Opens in new window.. The Alliance will be providing additional, in-depth articles outlining the success of each HTA winner in the coming months. The intent is to share employer-specific strategies in achieving high-value health care and to promote them to our membership so other employers will gain an opportunity to emulate their successes. Here were this year’s winners:
- WHIO (Wisconsin Health Information Organization). External Link. Opens in new window.
- Traci Rothenburger, Clinic Manager at Nordic PrivateCare. External Link. Opens in new window.
- Matt Ohrt, Director of Benefits/HR at Merrill Steel. External Link. Opens in new window.
- Tena Hoag, CFO at Advanced Laser. External Link. Opens in new window.
To watch the event in its entirety, please click here. External Link. Opens in new window..
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]







