
The Top Healthcare Trends Hurting Employers in 2022
Since the onset of the pandemic, price transparency has been one of the hottest healthcare trends, and we’ve kept close watch. (After all, Transparency isn’t just a healthcare trend, it’s one of our four core drivers of High-Value Health Care.)
However, as 2021 comes to a close, employers should keep their eye on a few other healthcare trends – including price transparency. Here are four healthcare trends that hurt employers and how they can be slowed heading into the new year.
Healthcare Trend #1: Spending is Going Up (And Has Been Since 1970)
Every person has a story to tell about an egregiously high healthcare bill (one of the most popular healthcare trends in and of itself) because prices have simply grown too high. Hospital prices have increased at a higher rate than the consumer price index, wages, and inflation.
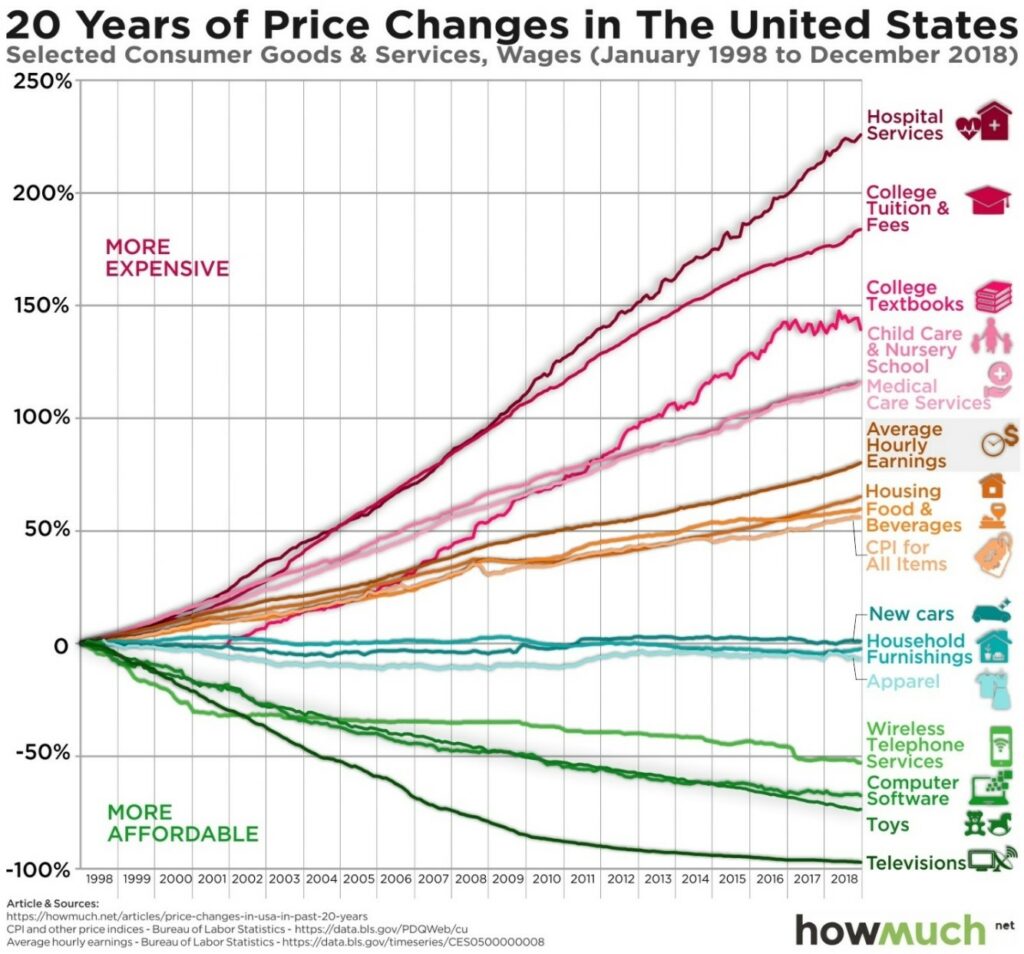
Over the past 40 years, the individual cost of healthcare – accounting for inflation – has increased six-fold. (In 2019 dollars, that’s an increase from $1,848 to $11,582.)
The trend of ever-increasing costs is especially bad for employers because they bear the brunt of it. Per Kaiser Family Foundation, employers paid 83% of their employees’ costs for single-coverage care in 2020, which was $10,340 per covered employee that same year.
If all 157 million Americans covered by their employer had single-coverage care, employers would collectively pay more than $1.6 trillion annually in healthcare costs. However, many employees opt for family-sponsored coverage, which employers pay 73% of and surpass $22,000 per family.
Slowing the trend: Pushing price transparency standards onto health systems is a good start, and perhaps the recently increased penalty for non-compliance will improve hospital participation.
Without having publicly available data on price, the healthcare marketplace cannot function properly. In a perfect world, prices for healthcare services would be widely available and easy to interpret, consumers could shop effectively, and providers would be forced to compete for their business – either by cost, quality, patient experience, or all of the above.
Healthcare Trend #2: Mergers Are Rising (And So Too Are Acquired Hospitals’ Prices)
In 2007, roughly half of all community hospitals belonged to a health system. A decade later, that number rose to two-thirds. This is one of those healthcare trends which can be attributed to the Affordable Care Act, the Affordable Care Act, which increased patient incentives to shift their healthcare utilization from an inpatient setting to an outpatient one. Hospitals moved quickly to capture those potential referrals through vertical integration.
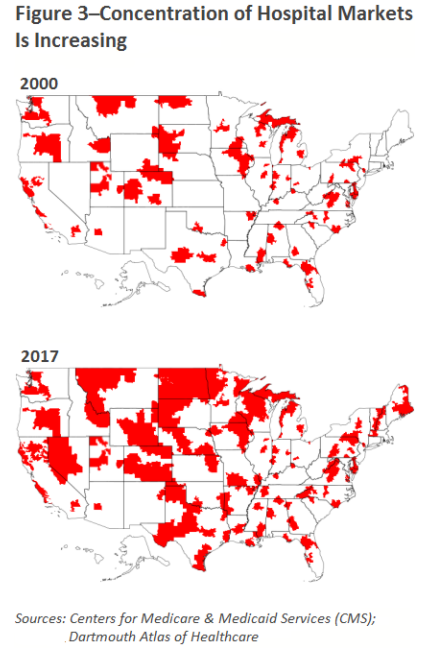
As we’ve previously written, hospital consolidation is not inherently a bad healthcare trend. Even if mergers don’t improve quality, they can actually reduce operating costs for the acquired hospitals by as much as 30%.
Those savings, however, have not historically translated into price decreases for consumers. In fact, after merging, hospital prices typically increase by 6-18%.
Slowing the trend: According to One Percent Steps, just a 10% reduction in hospital market concentration could lower hospital prices by $25 billion annually.
Healthcare Trend #3: As Healthcare Costs Rise, Quality Remains Stagnant
Health systems and hospitals have explained rising costs as a means to improve quality, (which has been effectively debunked,) while additional rationale used to justify high costs include:
- Low Medicare reimbursement
- Differences in patient mixes
- Variances in state-level funding.
First, despite charging commercial payers 247% more than Medicare, there’s no evidence hospitals need to set higher prices to make up for “uncompensated care.”
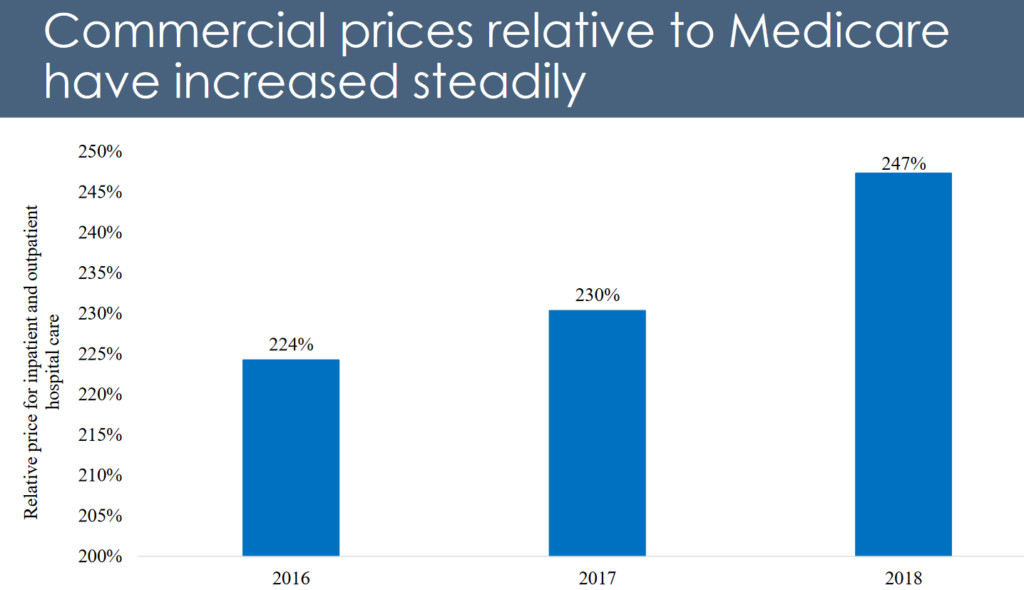
Additionally, RAND Corporation’s Hospital Price Transparency Project found no correlation between hospital prices and public health funding. In other words, states with more public funding don’t necessarily charge lower prices.
In that same analysis, RAND concluded that the differences across patient mixes do not explain price variations – which can happen for the same procedure in the same area.
Slowing the trend: To improve quality, we must encourage providers to move away from the traditional fee-for-service payment model. Payment reform that supports value-based methodologies, which shift some financial risk back to providers, will encourage health systems to improve their standards of care and compete for customers using quality metrics.
For example, Reference-Based Contracting by The Alliance® pays providers based on a percentage of Medicare, the single largest purchaser of healthcare in the United States. This benchmark brings forward the baseline employers need to pay fairer prices.
Healthcare Trend #4: Non-Profits Are Providing Less Charity Care & Suing More Patients
Non-profit community hospitals (which make up 92% of Wisconsin hospitals and 79% of Illinois hospitals,) are required to provide charity care and other community benefits in return for tax exemptions. Those tax breaks, funded by American taxpayers, are equivocal to $30 billion.
Despite that financial reprieve, some hospitals claim they must charge payers more to cost-shift the high amounts of charity care they provide.
But the numbers tell a different story: non-profit hospitals spent just 2.3% of their total facility expenses on charity care. That’s lower than government hospitals (4.1%) and for-profit hospitals (3.8%). It’s unsurprising then that seven of the top 10 most profitable hospitals are non-profits.
Even more disheartening is the fact that non-profit, charitable hospitals are increasingly suing patients over unpaid bills. In Wisconsin, Health Affairs discovered a 37% increase in hospital lawsuits from 2001 to 2018. That same analysis also found that non-profit hospitals were more likely to sue their patients than for-profit hospitals.
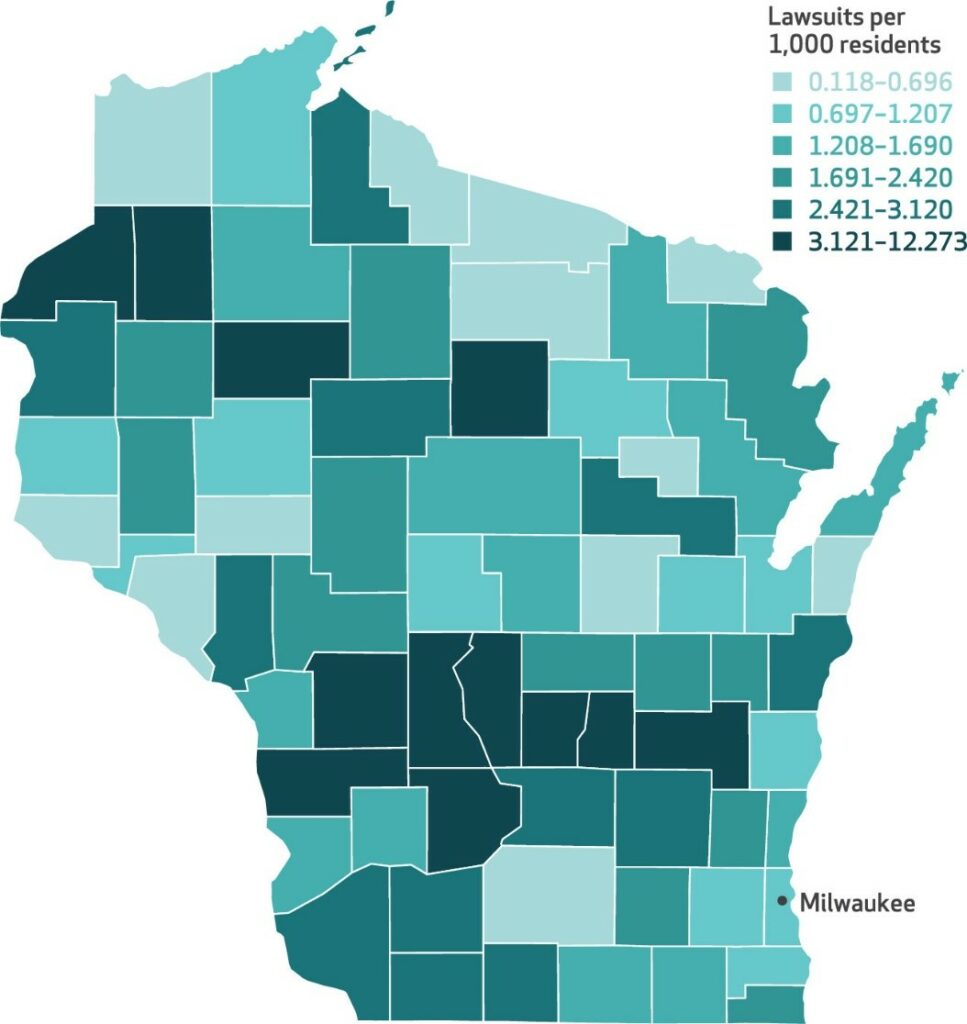
By using lawsuits to collect medical debt, hospitals discourage low-income employees, especially those from communities of color, from utilizing healthcare resources.
Slowing the trend: Publicly ranking hospitals based on the amount of charity care they provide would create a more transparent marketplace for consumers. Another option would be to back rules that enforce a minimum requirement of charity care for non-profit hospitals, or by loosening restrictions on who qualifies for charity care. Employers can also support health policy that disincentivizes hospitals from suing low-income patients.
Become a Part of Better Healthcare Trends
We’ve dedicated this article to healthcare trends that are hurting employers, but The Alliance has a more positive outlook on the New Year because we know what’s on the horizon; when employers band together and lead the way to push healthcare forward, we’re a powerful force.
As the voice for more than 300 self-funded employers, our cooperative serves as a trendsetter in health-purchasing. We approach benefit plan design with a level of passion that’s unmatched, and when it comes to provider networks, we custom-tailor Smarter Networks to suit the unique needs of every employer. Nobody is more committed to its clients than The Alliance, because The Alliance is a cooperative that’s owned by its clients.
To learn more about self insured health plans, check out our Smarter Self-Funded Health Plans page.








