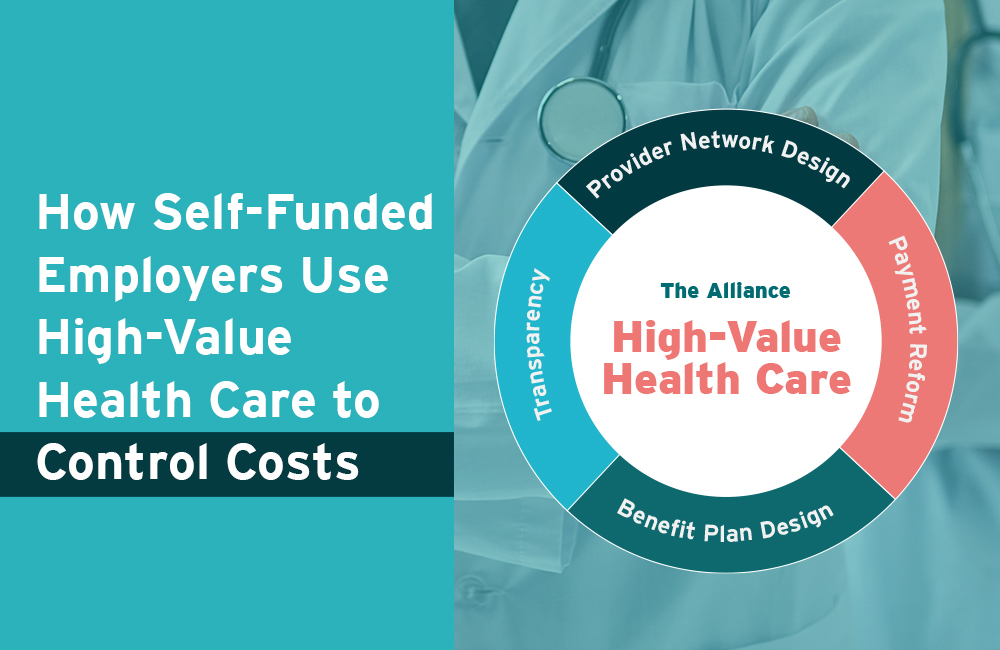
How Self-Funded Employers Use High-Value Health Care to Control Costs
The healthcare landscape is changing, and employers are driving that change. External Link. Opens in new window. through High-Value Healthcare. As a recent PBGH-KFF survey. External Link. Opens in new window. uncovered, 87% of employers believe that the current healthcare system is unsustainable, and now the government is starting to take notice. External Link. Opens in new window..
It’s no longer feasible for employers to pay increasingly high premiums – which reached more than $20,000. External Link. Opens in new window. per employee-sponsored family in 2019 – while raising their employees’ deductibles year after year. After all, employers want to provide high wages, good benefits, and high-quality healthcare to their employees. So, if employers care about their employees, brokers care about their employers, and health systems care about their patients, how can we put a stop to ever-increasing healthcare costs while offering higher-quality care at the same time? The $394 million answer is to utilize High-Value Healthcare.
The Four Core Drivers of High-Value Health Care
If you’re looking for a basic definition, High-Value Healthcare is high-quality, low-cost care. However, at The Alliance, we take that basic definition a step further to include improved access to high-quality, low-cost care. The Alliance is working to turn this ideology into practice through four strategies – what we call our Four Core Drivers of High-Value Healthcare: Transparency, Benefit Plan Design, Provider Network Design, and Payment Reform.
Transparency
First and foremost, transparency in healthcare is key. As our President & CEO, Cheryl DeMars, likes to remind us: “You can’t manage what you can’t measure.” To find a recent, notable study that shows the power of transparency, look no further than RAND Corporation’s Hospital Price Transparency Study. It displays the prices commercial consumers were paying nationwide for hospital services compared to what Medicare paid. The results of the study were jarring – especially in Wisconsin and Illinois – where employers are continually paying 2.5 to 3.5 times more than Medicare for the same services.
That study was critical in providing us and other group-purchasers with hard data that we can take to legislators to ask for help. (After all – employers cannot fix the healthcare system alone. External Link. Opens in new window..) Driven by the study’s data – and bi-partisan calls from consumers – both the Trump and Biden administrations signed a slew of executive orders aimed at increasing transparency in healthcare.
Though the effectiveness of the resulting federal regulations is still being determined, they are certainly moving price transparency in the right direction. In fact, The Alliance used the data supplied by hospitals complying with federal law to compare our rates with our competitors. The results reaffirmed why insurers and hospital systems benefit from secret prices – and why self-funded employers all across the Midwest join our cooperative – our rates are significantly lower. External Link. Opens in new window..
Provider Network Design
In a healthcare landscape where providers are shrinking due to hospital consolidation and mergers, The Alliance is continually growing to ensure convenient access to high-value care for our employer-members. Our Smarter Networks℠ are comprised of several high-performing provider networks that drive employers to save through smart innovation.
Here’s how Provider Network Design works: The Alliance contracts directly with providers on behalf of our pooled purchasing power – 340+ employers strong – to negotiate lower rates. Our custom provider networks have grown to 38,000 clinicians, and we’ve strategically evolved (see our partnership with Trilogy Health Networks. External Link. Opens in new window.) to offer employers unprecedented access to high-value care across the Midwest.
Payment Reform
Traditionally, in healthcare, providers are paid on a fee-for-service basis. This produces expensive, (sometimes unnecessary) referrals, low patient engagement, and poor health outcomes. The Alliance contracts differently. We align financial incentives that reward providers for high-quality, low-cost care and leverage our large purchasing power to create unique contract provisions that protect employers where other insurers can’t. Our value-based payment methodology includes inflation controls and some protection against hospital consolidation.
Additionally, through Reference-Based Contracting by The Alliance®, we contract rates as a percent of Medicare which gives self-funded employers the benchmark necessary to pay fair prices for healthcare services. Reference-Based Contracting moves some of the risk traditionally retained by employers onto providers by using a total cost of care methodology rather than a discount.
Benefit Plan Design
Strategic benefit plan design brings together all four core drivers by incentivizing employees to choose high-value care – which saves them and their employer money. Just one example: some of our employer-members pay their employees cash incentives for having a test or procedure done at a particular provider. Why? Because pricing can vary wildly from provider to provider, employers can afford to pay their employees hundreds – sometimes thousands – of dollars to use a provider that offers the same (if not, better) quality, but at a much lower cost.
And if you recall the section about designing provider networks that offer a wide range of high-value providers, you can understand how good benefit design means tiering networks to nudge employees to lower-cost providers.
For example, if an employer owns or shares a Direct Primary Care clinic. External Link. Opens in new window., they can offer a plethora of no-cost services through it. That same employer can offer preferred pricing at a health system of their choosing for services not covered at the clinic. They may pay a co-pay to the system that’s lower than other options but higher than at their clinic. Benefit plan design like this encourages employees to make smarter decisions that save them – and the plan – money. Our tiered network option, The Alliance Premier Network, offers employers total control with up to four tiers to customize their health plan.
Join a Cooperative Driven by High-Value Health Care
To learn more about self insured health plans, check out our Smarter Self-Funded Health Plans page or email me – I’d love to answer your questions!








